Ureaplasma : A Common Yet Often Missed Infection
Ureaplasma is one of the most common bacteria found in the human urogenital tract, yet it remains one of the most misunderstood and frequently undiagnosed causes of persistent discomfort. Belonging to the Mycoplasma family, Ureaplasma is unique because it lacks a cell wall, which makes it resistant to common antibiotics like penicillin. For sexually active individuals, understanding this pathogen is crucial, as local and regional data indicate it is highly prevalent and becoming increasingly difficult to treat due to rising antibiotic resistance.
What is Ureaplasma?
Ureaplasma is a genus of tiny bacteria that normally reside in the mucous membranes of the urinary and reproductive tracts. The two species that infect humans are Ureaplasma urealyticum (Uu) and Ureaplasma parvum (Up)1. They are often grouped together as Ureaplasma species (spp.).
A key point of confusion is that finding Ureaplasma does not automatically mean you have an infection that requires treatment. It is estimated that a significant portion of the sexually active population carries these bacteria without any symptoms2. Problems arise when the bacterial load becomes too high or the body's immune defences are lowered, potentially leading to inflammation and infection.
Why Ureaplasma Matters for Hong Kong
Recent scientific studies from our region paint a clear picture of why Ureaplasa is a relevant health consideration.
- High Prevalence: A major 2025 study of over 47,000 patients in Eastern China found that genital mycoplasmas (primarily Ureaplasma) were detected in 43.74% of suspected cases. Pure Ureaplasma spp. infection accounted for 37.00% of this total3.
- Demographic Trends: The same study found infection rates were significantly higher in females (44.00%) than in males (20.12%), and the highest rate was observed in the youngest age group (under 21 years)3.
- A Serious Treatment Challenge: Perhaps the most critical finding is the alarming rate of antibiotic resistance. The study reported that Ureaplasma showed an 83.39% resistance rate to ciprofloxacin and 66.34% to ofloxacin, two commonly used fluoroquinolone antibiotics, with resistance increasing yearly3.
The table below summarizes these key findings from the regional data:
| Aspect | Key Statistic | Implication for Hong Kong |
|---|---|---|
| Overall Detection Rate | 43.74% in symptomatic patients3 | Ureaplasma is a very common finding in clinics. |
| Pure Ureaplasma Rate | 37.00%3 | It is the dominant genital mycoplasma. |
| Gender Disparity | 44.00% in females vs. 20.12% in males3 | Women are more than twice as likely to be diagnosed. |
| Ciprofloxacin Resistance | 83.39%3 | This common antibiotic is largely ineffective. |
Symptoms: Often Silent, Sometimes Troublesome
Many people with Ureaplasma experience no symptoms at all. When symptoms do occur, they are often non-specific and can be mistaken for other common conditions like a urinary tract infection (UTI) or typical vaginitis/cervicitis.
Common symptoms in both men and women may include:
- Burning or stinging sensation during urination.
- Unusual genital discharge.
- Lower abdominal or pelvic pain.
- Redness or discomfort in the genital area.
Gender-Specific Concerns:
- In Men: Ureaplasma is a known cause of non-gonococcal urethritis (NGU), which is inflammation of the urethra not caused by gonorrhoea. It has also been controversially linked to prostatitis and potential impacts on sperm quality and male infertility.
- In Women: Beyond urethritis, it is associated with bacterial vaginosis (BV), cervicitis, and pelvic inflammatory disease (PID). Most significantly, it is a recognized cause of adverse pregnancy outcomes, including chorioamnionitis, preterm premature rupture of membranes, and preterm birth.
Complications and Health Risks
If left untreated, a symptomatic Ureaplasma infection can lead to more serious health issues:
- Increased Susceptibility: The infection can make individuals more vulnerable to acquiring other sexually transmitted infections (STIs), including HIV.
- Chronic Pain: It can contribute to chronic pelvic pain and persistent urethral discomfort.
- Reproductive Health: As noted, associations with infertility in men and pregnancy complications in women are significant concerns.
- Disseminated Infection: In rare cases, particularly in immunocompromised individuals (e.g., transplant recipients), it can cause severe systemic infections.
Diagnosis: Getting the Right Test in Hong Kong
Ureaplasma will not show up on a standard urine culture or STI panel. It requires specific testing.
- Test Type: The most accurate and recommended method is a Nucleic Acid Amplification Test (NAAT), such as a PCR test, which detects bacterial DNA. This can distinguish between Uu and Up. Traditional culture with antibiotic susceptibility testing is also available and useful for guiding treatment.
- Sample Collection: Testing is done using a first-void urine sample or a genital swab.
- Where to Test: In Hong Kong, several private clinics and laboratories offer specific Ureaplasma testing. For example, targeted PCR tests are available, with results often in 8-24 hours.
Treatment and the Critical Challenge of Resistance
Treatment is not always required for asymptomatic carriage. However, it is strongly recommended for individuals with symptoms, for infertile couples where Ureaplasma is detected, and for pregnant women with a history of preterm birth.
The central challenge is antibiotic resistance. Due to its lack of a cell wall, Ureaplasma is only susceptible to antibiotics that inhibit protein or DNA synthesis.
| Antibiotic Class | Example Drugs | Current Efficacy & Notes |
|---|---|---|
| Tetracyclines | Doxycycline, Tetracycline | Generally remain effective. Often used as first-line treatment. Resistance rates are relatively low in regional studies. |
| Macrolides | Azithromycin, Josamycin, Clarithromycin | Variable efficacy. Azithromycin is commonly used, but resistance is a growing global concern. Josamycin showed low resistance in the 2025 China study. |
| Fluoroquinolones | Ciprofloxacin, Ofloxacin, Levofloxacin | High Resistance. NOT recommended as first-line. Studies show resistance rates exceeding 66-83% in our region. |
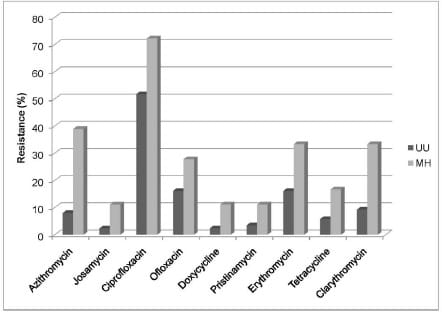
Drug Resistance of Ureaplasma
There were considerable differences in levels of resistance to the antibacterial agents for the two bacterial species. However, the MH strains showed generally higher resistance rates than UU ones.
- For MH, the highest resistance rates were registered for ciprofloxacin (77.27%), followed by macrolides (azithromycin 38.88%, clarythromycin and erythromycin - 33.33% each) and ofloxacin (27.77%). Lower resistance rates (p=0.028) were registered for tetracycline, josamycin, pristinamycin, and doxycycline, i.e. 16.66%, 11.11%, 11.11%, and 11.11% respectively.
- For UU isolates, the ciprofloxacin resistance was also very high (51.72%), while the resistance rates to the other tested antibiotics were significantly lower (p=0.022), i.e. ofloxacin (16.09%), erythromycin (16.09%), clarythromycin (9.19%%), azithromycin (8.05%), tetracycline (5.75%), pristinamycin (3.45%), josamycin (2.30%) and doxycycline (2.30%)
Key Treatment Principles:
- Antibiotic Sensitivity Testing: Given the high and variable resistance, an antibiotic susceptibility test (from a culture) is ideal to guide therapy, especially for persistent or recurrent infections.
- Partner Treatment: To prevent "ping-pong" reinfection, all sexual partners must be tested and treated simultaneously, even if they have no symptoms.
- Test of Cure: A follow-up test (recommended at least 3-4 weeks after completing antibiotics) is advised to confirm the infection has cleared.
Conclusion and Recommendations for Hong Kong Residents
Ureaplasma is a highly prevalent, often asymptomatic organism that can become a pathogenic source of persistent urogenital symptoms and serious reproductive complications. The alarming rise in antibiotic resistance, particularly to fluoroquinolones, makes accurate diagnosis and guided treatment essential.
If you are experiencing unexplained urinary or genital symptoms that have not resolved with standard treatments, or if you have concerns regarding fertility or pregnancy history, discuss Ureaplasma testing with your doctor. Seek clinics in Hong Kong that offer specific NAAT (PCR) testing or culture with sensitivity to ensure you receive a correct diagnosis and an effective, tailored treatment plan.
Ref:
- Beeton ML, Payne MS, Jones L. The Role of Ureaplasma spp. in the Development of Nongonococcal Urethritis and Infertility among Men. Clin Microbiol Rev. 2019 Jul 3
- Ureaplasma Urealyticum/ Ureaplasma Parvum (UU/UP): An Emerging Resistant Pathogen with Potential Severe Consequences. BY: Dr. Wong Tin Yau, Andrew
- Zhang YQ, Su N, Huang L, Xu WD, Wang YN, Gao JJ. Emerging resistance in genital mycoplasmas: 6-year trends of Ureaplasma spp. and Mycoplasma hominis infections in Eastern China. BMC Infect Dis. 2025 Oct 31
- Waites KB, Katz B, Schelonka RL (2005) Mycoplasmas and ureaplasmas as neonatal pathogens. Clin Microbiol Rev 18:757–789. doi:10.1128/CMR.18.4.757-789.2005)
- (REF: Glass JI, Lefkowitz EJ, Glass JS, Heiner CR, Chen EY et al (2000) The complete sequence of the mucosal pathogen Ureaplasma urealyticum. Nature 407:757–762. doi:10.1038/35037619. )
- REF: Association of Ureaplasma urealyticum (Biovar 2) With Nongonococcal Urethritis, 2004. https://journals.lww.com/stdjournal/Fulltext/2004/03000/Trends_in_the_Prevalence_of_Pathogens_Causing.11.aspx ).
- (REF: The Role of Ureaplasma spp. in the Development of Nongonococcal Urethritis and Infertility among Men. 2019. https://pubmed.ncbi.nlm.nih.gov/31270127/)
- (ref: A Case of Rectal Ureaplasma Infection and Implications for Testing in Young Men Who Have Sex with Men: The P18 Cohort Study, 2017. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5374866/#B4 ).
(Text Only)

